When it comes to the health of your lower back, spinal discs are a must. They cushion the impact of movement between the spine's bones, provide structural support for the trunk, and enable a wide range of motion.
On the other hand, if a disc herniates and some of its inner material leaks out, it can quickly switch from being helpful to irritating, leading to back pain and possibly pain and nerve sensations down the leg.
Most of the time, the symptoms of a herniated disc start for no apparent reason. Or they can happen when someone lifts something heavy or twists their lower back, putting extra pressure on the discs.
Herniated discs in the lower back are a common medical problem that affects most people between the ages of 35 and 50.
This article talks about how a herniated disc in the lower back happens, how it is diagnosed, and the surgical and non-surgical ways to treat it.
The gel-like centre of each disc, called the nucleus pulposus, is protected by a rigid ring called the annulus.
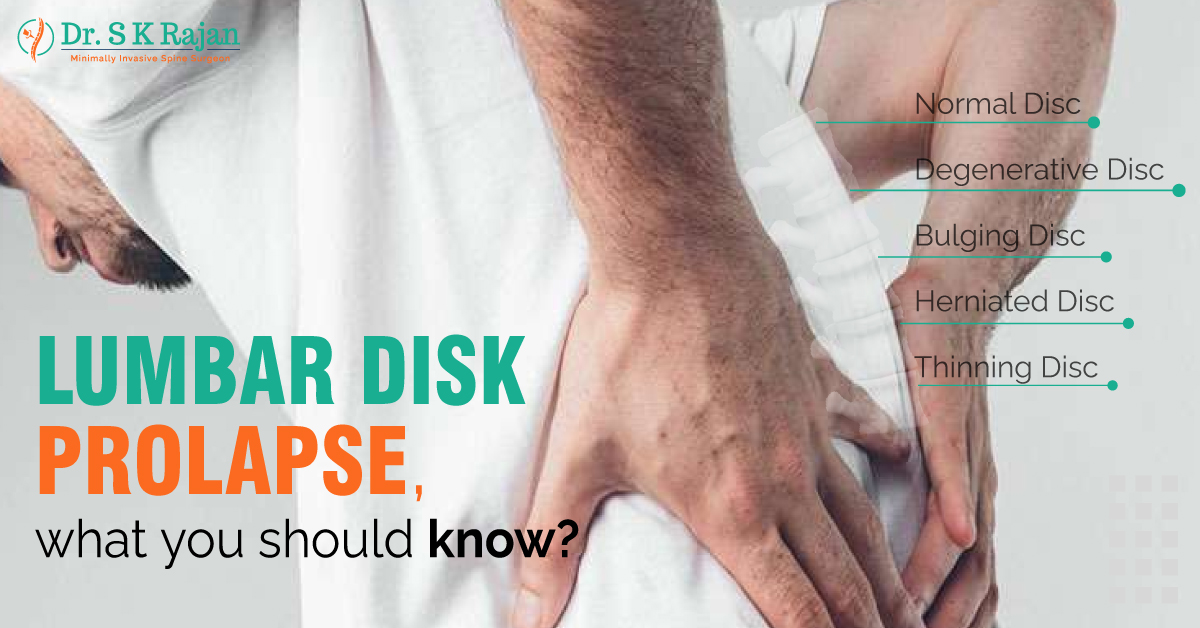
As the discs age and wear down from everyday use, they lose some of the fluid that makes them soft and spongy. Because of this, the discs tend to flatten out and get more complicated. Disc degeneration is a gradual process that manifests itself in early adulthood, on imaging studies, but originates in childhood.
The disc's outer ring can crack, bulge, or rupture if the spine is under undue stress. If this happens in the lower back (the lumbar spine), the bulging disc may put pressure on a spinal nerve root in the area. Or, the nerve may be hurt by something inside the body that causes inflammation. The pain shoots up and down the leg and into the buttock.
A doctor may tell a person with a herniated lumbar disc that it happened because of degenerative disc disease. This word can be scary and lead people astray. Degenerative disc disease isn't a disease that gets worse over time, and it doesn't always cause problems that last for a long time.
Even though age is the most common risk factor, being inactive can weaken the back and abdominal muscles, which may not support the spine as well as they should. Back injuries also happen more often when people who aren't usually physically active do things that are
too hard. Back injuries can also occur on the job if you have to lift heavy items or twist your back.
The symptoms of lumbar disc disease depend on where the disc has herniated and what nerve root it is pressing on. Most people with lumbar disc disease have these signs:
Back pain that comes and goes or is always there. This can worsen when you move, sneeze, cough, or stand for a long time. Muscle spasms in the back Sciatica is pain that starts in the back or buttock and goes down the leg to the calf or foot. Decreased reflexes at the knee or ankle, weakness in the legs, numb leg or foot, and changes in how the bladder or bowels work are also sciatica symptoms. Lumbar disc disease can cause symptoms similar to, but not necessarily indicative of, other diseases or medical problems. Always see your doctor to find out what's wrong.You may need to undergo one or more of the following tests in addition to a thorough medical history and physical examination:
At least 80 or 90% of disc prolapses get better on their own, and almost all symptoms disappear. Most of the time, this takes 6–8 weeks, but it could take longer.
Unless there is evidence of substantial spinal cord or nerve root compression or poor function, conservative treatment is typically the first line of defence for acute disc prolapses. Most of the time, a combination of anti-inflammatory and paracetamol-based medicines, a physiotherapy programme and sometimes hydrotherapy and pilates are recommended.
If the symptoms don't go away after reasonable conservative treatment, it may be suggested to do something more. This could involve surgery or an injection of a local anaesthetic into the nerve sheath. Steroids have not been shown to help more. Surgery has been indicated to help people get better faster after a slipped disc.
The treatment given to each person will differ based on their appearance, what the x-rays show, and other factors.
Your neurosurgeon or spinal surgeon will make a treatment plan for you based on your specific situation, and this plan will be checked on from time to time.